 UND’s principal investigator is
Catherine A. Brissette, PhD, an assistant professor in the Department of Biomedical Sciences at the UND School of Medicine and Health Sciences. She has received a $108,000 grant from the
Global Lyme Alliance, which funds research for Lyme and tick-borne disease research. She serves on the alliance’s advisory board, which serves to peer review grants in a manner similar to the National Institutes of Health. Archana Dhasarathy, PhD, and John Watt, PhD, in the SMHS Department of Biomedical Sciences are collaborating with Brissette in the research. “Our preliminary data suggest that
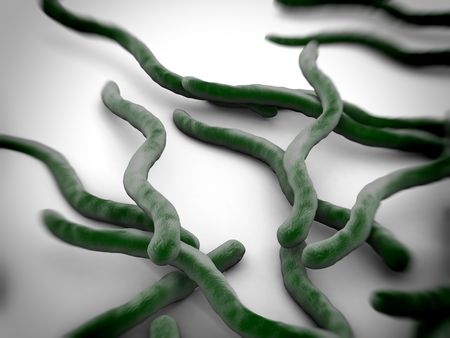
Bb induces substantial changes in epigenetic factors in human astrocytes,” said Brissette. “Astrocytes are critical components of the blood-brain barrier; these cells are key responders following a central nervous system injury or an infection like Lyme disease.” The blood-brain barrier is a semipermeable membrane that protects the brain from foreign substances by allowing only some materials to enter the brain from the bloodstream. However, the barrier can be breached by infectious agents like the
Bb bacterium. “We hypothesized that neurological symptoms from Lyme disease are perpetuated by
Bb-induced epigenetic changes that lead to persistent neuroinflammation,” Brissette said. Neuroinflammation is damaging inflammation of nervous tissue from a traumatic brain injury, an infection such as Lyme disease, and other “insults” or injuries. In their studies of neuroborreliosis, the disorder of the central nervous system caused by Bb infection, Brissette, her SMHS colleague Thad Rosenberger, and other biomedical scientists have shown that Bb-induced neuroinflammation can be reversed by supplementing the diet of their animal model with acetate. In the brain, acetate is converted to a substance that is a widely active precursor in numerous biological processes and as a substrate for a process that leads to changes in gene expression.
Read the entire article on Outbreak News Today.
UND’s principal investigator is
Catherine A. Brissette, PhD, an assistant professor in the Department of Biomedical Sciences at the UND School of Medicine and Health Sciences. She has received a $108,000 grant from the
Global Lyme Alliance, which funds research for Lyme and tick-borne disease research. She serves on the alliance’s advisory board, which serves to peer review grants in a manner similar to the National Institutes of Health. Archana Dhasarathy, PhD, and John Watt, PhD, in the SMHS Department of Biomedical Sciences are collaborating with Brissette in the research. “Our preliminary data suggest that
Bb induces substantial changes in epigenetic factors in human astrocytes,” said Brissette. “Astrocytes are critical components of the blood-brain barrier; these cells are key responders following a central nervous system injury or an infection like Lyme disease.” The blood-brain barrier is a semipermeable membrane that protects the brain from foreign substances by allowing only some materials to enter the brain from the bloodstream. However, the barrier can be breached by infectious agents like the
Bb bacterium. “We hypothesized that neurological symptoms from Lyme disease are perpetuated by
Bb-induced epigenetic changes that lead to persistent neuroinflammation,” Brissette said. Neuroinflammation is damaging inflammation of nervous tissue from a traumatic brain injury, an infection such as Lyme disease, and other “insults” or injuries. In their studies of neuroborreliosis, the disorder of the central nervous system caused by Bb infection, Brissette, her SMHS colleague Thad Rosenberger, and other biomedical scientists have shown that Bb-induced neuroinflammation can be reversed by supplementing the diet of their animal model with acetate. In the brain, acetate is converted to a substance that is a widely active precursor in numerous biological processes and as a substrate for a process that leads to changes in gene expression.
Read the entire article on Outbreak News Today.




-2.jpg)


